Kidneys and Ureters
The kidneys perform several functions. They filter waste products out of the blood, and turn them into urine. They also produce several important hormones that regulate blood pressure, red blood cell production and calcium.
Urine is full of minerals and proteins that are excreted by the kidneys. When there are too many of one of these (e.g. calcium), or there is too little water to dissolve them (e.g. dehydration), they can crystallize out and turn into 'stones' in the kidneys. Some people are genetically prone to forming stones, whilst others have underlying medical diseases that can cause them. The majority of people do not however, and diet and fluid intake, as well as geography can play a role. 1 in 8 men and 1 in 10 women will have a stone in their lifetime and they are hugely on the increase in the western world. There is a 50% chance of recurrent stones at 10 years.
There are several different types of stones including: calcium oxalate, calcium phosphate, uric acid, struvite (infection stones), cystine and drug related.
Once stones have formed they can either sit in the kidney, or travel down the ureters, sometimes getting stuck. Kidney stones can cause significant symptoms such as pain (colic), blood in the urine, urine infections and nausea and vomiting. Pain from stones is often described as severe, and may sometimes lead to an emergency attendance to accident and emergency.
Conservative:
Many stones that are travelling down the ureters will pass spontaneously (90%). In general the smaller they are (<5mm), the more likely they are to pass, albeit this can be very painful. Strong painkillers are usually prescribed to help with symptoms and to allow patients to go home, whilst nature takes its course. You may be prescribed a tablet called tamsulosin to relax the ureters and aid stone passage. It is vital that patients are followed up by a urologist, to ensure that the stone has passed. This is normally done with an x-ray or CT scan. It can take 4-6 weeks for a stone to pass. There are certain instances when it is not safe to continue with conservative management:
- When there is also a urine infection
- When the pain is not controllable
- When there is kidney failure or a single kidney
- When stones are very large
In these circumstances it is usual to drain the kidney with either a hollow tube internally called a stent, or externally through the back (nephrostomy tube).
Extracorporeal lithotripsy (ESWL):
ESWL can be used as an emergency treatment for stones that are stuck in the ureter or as elective treatment for most kidney stones up to 2cm in size. It has been in use for 30 years and is regarded as a safe and effective treatment, with clearance rates of up to 90% reported. It is an outpatient procedure, administered with simple oral analgesia or EntoNox gas. The treatment lasts for 30 minutes, and it is often necessary to repeat it 2-4 weeks later.
The treatment involves lying on special table called a lithotripter. A cushion is placed against the patients back, and sound waves are focused onto to the stone using either ultrasound or x-rays. The stone is broken up into fine dust that is then passed painlessly out in the urine. It can be uncomfortable during the procedure but this stops as soon the process is finished. About 5-10% of patients get pain as larger fragments pass through.
Most urology centers do not have emergency access to ESWL, but here in Brighton and Sussex Urology we have access to the only machine is Sussex that is able to provide next day emergency treatment. This is based in Hayward's Heath.
Download an ESWL information sheet

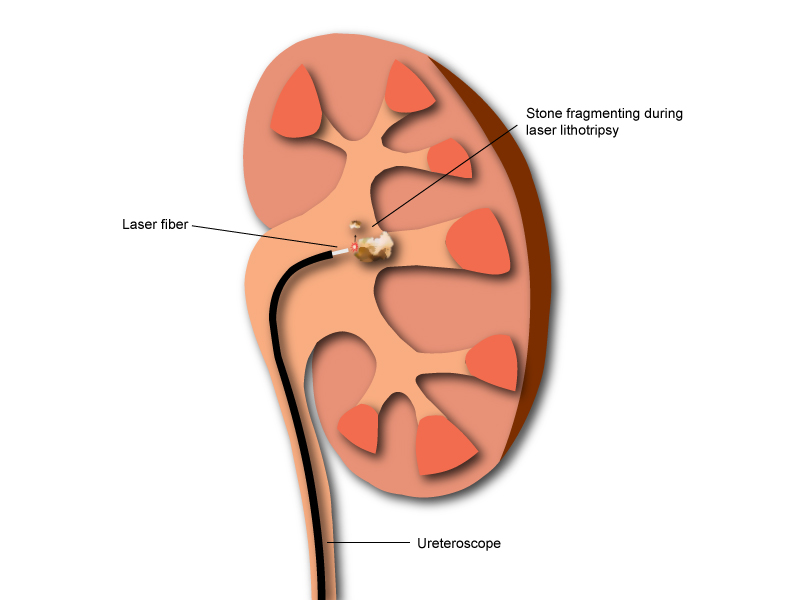
ESWL is not suitable for all kidney and ureteric stones. With improving technology and the miniaturization of endoscopes it is now possible to treat stones with fine telescopes passed up through the urethra, bladder and ureters, and for stones to be broken up with lasers (lasertripsy) and removed with small baskets. This operation is called a ureteroscopy and over the past 10 years has been increasingly gaining ground as a fallback or alternative to ESWL. It is performed under general anaesthesia, but is usually a day case procedure, and the recovery is quick as there are no 'cuts' involved. It is a very safe procedure with few side effects. Occasionally the ureter is tight, and will not allow passage of the ureteroscope. In this situation it is necessary to leave a temporary ureteric stent for 2 weeks. This allows for dilation of the ureter making a subsequent procedure easier.
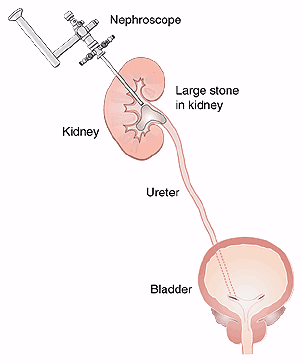
For stones that are larger than 2cm, or related to infection (staghorn stones), or that sit in a kidney with abnormal anatomy, the gold standard procedure is called a percutaneous nephrolithotomy (PCNL). This is performed under general anaesthesia, and involves a small incision in the back, followed by the passage of a telescope into the kidney to remove stones. It is minimally invasive, and normally entails a 2-day stay in hospital afterwards. It allows for the largest of stones to be removed, to the extent that open stone surgery has all but disappeared. There are risks of bleeding and infection afterwards and it should only be performed by an expert in stone surgery. Increasingly PCNL is being used for smaller stones using specialized miniaturized equipment – mini-PCNL.
It is helpful to send off any stone that has passed for analysis. In addition you may be advised to have some blood and urine tests to investigate why you have formed a stone. There are some medications that can be prescribed to cut down the future risk of another stone.
General advice for preventing stones is:
- Maintain a high fluid intake (>2 litres water a day)
- Cut down salt intake
- Low protein diet
- A normal calcium intake
- Avoid black tea (breakfast tea) – put milk in
- Reduce intake of oxalate containing foods: chocolate, rhubarb, spinach, nuts, beetroot, tomato juice
- High intake of citrate (citrus fruits such as oranges and lemons)
There are 2 areas that kidney tumours can grow. Either in the meat of the kidney where blood is filtered, or in the collecting system of the kidney were urine is collected before it drains down the ureters.
Tumours that form in the meat of the kidney can be benign or malignant. Kidney (renal cell) cancer is increasing, partly because it is increasingly being picked up at an early stage when scans are done to diagnose other conditions in the abdomen (an incidental finding). Classically kidney cancers present with blood in the urine, a palpable lump in the abdomen, and pain in the flank.
The investigation of choice is a CT scan, but you may be asked to have a biopsy or even an ultrasound to help decide whether they are cancerous or not.
Treatment normally involves removal of part or the whole of the affected kidney. This can be done as a keyhole operation.
Tumours that form in the collecting system of the kidney (transitional cell cancer) usually present with blood in the urine, and are often associated with smoking. Along with a CT scan it is usually necessary to look up into the kidney (ureteroscopy) to confirm the diagnosis. Treatment involves removal of the affected kidney and ureter, although it is sometimes possible to laser tumours at the time of ureteroscopy. The upside is preservation of the kidney and avoidance of a major operation; the downside is frequent check ups involving general anaesthesia and ureteroscopy, and the potential for recurrence.




