The Prostate
The prostate is a small walnut shaped gland that sits in front of the bladder. The urethra travels through the middle of the prostate. It has 2 functions:
- It produces around 30% of the overall volume of seminal fluid. This contains nutrients for semen.
- It acts as a muscular pump aiding in ejaculation
Prostate cancer is the most common cancer diagnosed in men in the UK, with over 40,000 new cases diagnosed every year. The causes of prostate cancer are largely unknown, but it is more common if you are of African or African-Caribbean descent, or if you have a first-degree male relative affected. It is usually symptomless at an early stage, but it may give local symptoms such as urinary symptoms, blood in the urine, retention of urine, or distant symptoms such as bone pain.
There is no single test to diagnose prostate cancer, but it is normally diagnosed with a blood test called PSA, a rectal examination of your prostate (DRE), and a biopsy. There are some excellent online resources to explore this complicated subject in more detail (www.nhs.uk).
PSA is only produced in the prostate, but its levels can be elevated with urine infections, benign enlargement of the prostate, prostatitis (inflammation in the prostate), as well as prostate cancer. A raised level can therefore lead to unnecessary anxiety. Using PSA to screen for prostate cancer is controversial and not recommended in the UK in men without symptoms (www.nhs.uk). There is however increasing evidence that a PSA test in a man in his late 40's or early 50's can stratify the risk of prostate cancer in later life. A raised PSA often leads to a prostate biopsy that is performed under local anaesthetic. This can lead to infection so antibiotics are normally prescribed.
The difficulty with prostate cancer is that some prostate cancers are almost certainly not dangerous. Being diagnosed with one can however lead to considerable anxiety and psychological harm. Without a biopsy we don't yet have the ability to distinguish which are harmful (and therefore need diagnosing), and which are irrelevant (which we don't need to diagnose). If there was a treatment that carried no side effects, then perhaps it wouldn't matter, but the 2 established treatments (surgery and radiotherapy), can be associated with impotence and incontinence.
To address these issues most urologists will use active surveillance to monitor these harmless cancers, without immediate treatment, and reserving intervention if the cancer shows potentially dangerous changes in the future. Utilizing this strategy 2/3rd men will avoid treatment, with the rest treated safely at a later date. This is a safe strategy.
For cancers that show more dangerous features the treatments available locally are surgery (radical prostatectomy which may be performed laparoscopically), external beam radiotherapy or brachytherapy. The decision as to which option is suitable is complex and needs a lengthy discussion with a surgeon and oncologist. There are online resources available to help (sdm.rightcare.nhs.uk).
When prostate cancer is advanced there are still several treatment options, which, whilst not curative, can extend survival by many years. It is often the case that this will be a disease that patients will live with, and die of something else eventually. The treatments revolve around cutting off the male hormone testosterone, usually with an injection every 3 months. There are several novel treatments becoming available including chemotherapy, abiraterone, enzalutamide, and viral vaccines.
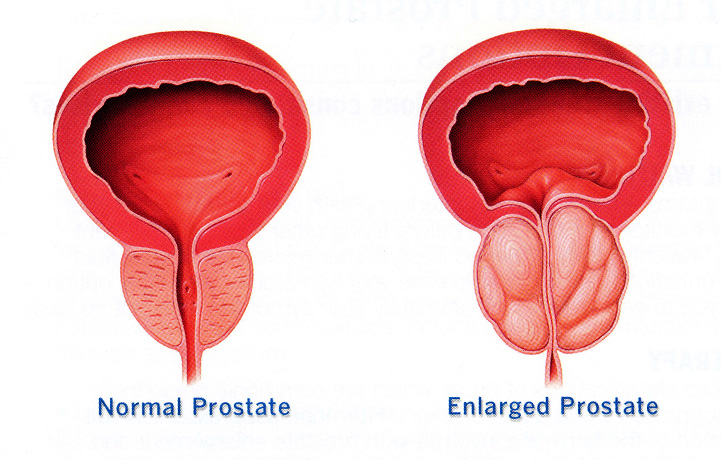
Most men will experience benign enlargement of their prostate (BPH) as they get older. It has been described as much a part of ageing as graying of the hair. This process starts in one's 30-40's, but symptoms usually present in one's 50's and 60's. The reasons behind this benign growth are not well understood. As the prostate grows it squeezes the urethra that carries urine through it, leading to a reduction in urinary stream. If severe this can lead to urinary retention (the inability to pass urine). As a consequence the bladder muscle has to work increasingly hard to eject urine, and it can become irritable as a result leading to urinary frequency and urgency (overactive bladder symptoms). Not everybody will experience these symptoms, but the following can occur:
- Poor flow
- Difficulty starting or stopping urinating
- Having to push or strain to start urinating
- The sensation of not having emptied completely
- Frequency
- Urgency
- Incontinence
- Getting up at night to pass urine
BPH is usually not life threatening, but can significantly affect your quality of life. A prostate symptom score sheet can help describe you symptoms.
Complications of this condition are rare but can include:
- Urinary retention
- Recurrent urinary tract infections
- Formation of bladder stones
- Severe blockage leading to kidney failure (very rare)
BPH is investigated with a patient history and examination, including an examination of the prostate. You will be asked to fill in a prostate symptom score sheet as well as a frequency volume chart (bladder diary). You may be asked to do a flow rate test (non-invasive) to assess how restricted your urinary stream is, followed by a simple ultrasound of your bladder to see if it is emptying properly. Finally you will have some simple blood tests and may be offered a PSA blood test.
Conservative treatment:
Not all men need treatment, but maybe seeking reassurance that this is not prostate cancer. In those cases where symptoms are mild, there are certain useful things that you can do to help:
- Avoid caffeinated drinks
- Double void, to try and empty you bladder completely
- Reduce you fluid intake in the evening
- Pass urine before going to bed
Medical (drug) treatment
There are several drugs that can be used to manage, not cure, this condition.
Alpha-blockers (tamsulosin, alfusozin, doxazosin etc) work by relaxing the muscle of the prostate, increasing urine flow, and should be the first line treatment. Patients usually notice an improvement with 48-72 hours. Side effects are few, and disappear on stopping the medication, and can include:
- Low blood pressure (dizziness on standing)
- Weakness
- Retrograde ejaculation
- Headache
- Nasal congestion
5 alpha-reductase inhibitors (finasteride, dutasteride) work by shrinking the prostate, and thus improving flow. They take up to 6 months to work and maybe prescribed in conjunction with an alpha-blocker. They are not as good as alpha-blockers at improving symptoms but may prevent the complications of BPH in men with big prostates (retention, need for surgery).
Complications include:
- Erectile dysfunction
- Loss of libido
Anticholinergic medication (solifenacin, tolterodine etc) is usually prescribed for patients with an overactive bladder. In men with symptoms from an enlarged prostate, they maybe used in conjunction with an alpha-blocker to reduce urinary frequency and urgency.
There are several herbal remedies on the market (saw palmetto), but the evidence for any benefit with these is weak.
There are several surgical approaches to the treatment of BPH. The gold standard remains the TURP (transurethral resection of prostate), but other surgical approaches include open prostatectomy, bladder neck incision (BNI) and minimally invasive approaches such as Greenlight laser prostatectomy. More recently a procedure called UroLift® has become available.
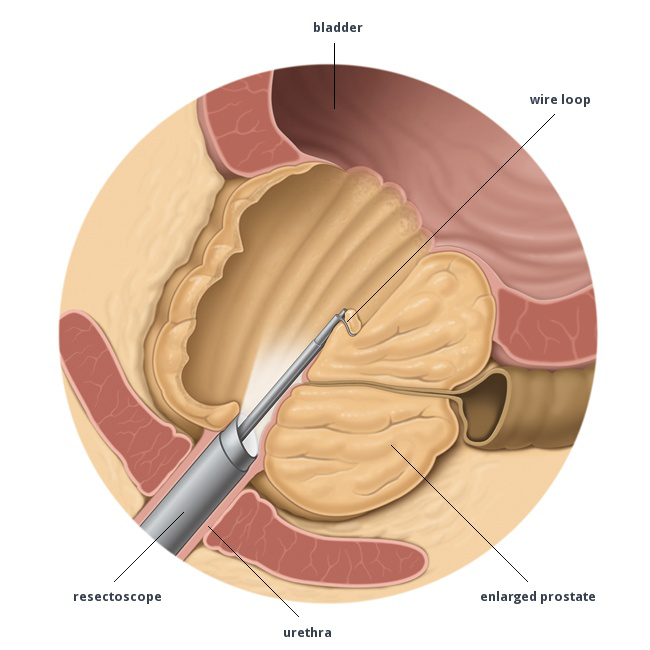
Transurethral resection of prostate (TURP)
A TURP is an operation in which an instrument (resectoscope) is inserted up the urethra (water pipe) and used to remove a part of the prostate that is blocking the flow of urine. You will be given either a general or a spinal anaesthetic for the procedure. The operation takes about 45 minutes and you will be in hospital for about two to three days.
Bladder neck incision
A TURP is an operation in which an instrument (resectoscope) is inserted up the urethra (water pipe) and used to remove a part of the prostate that is blocking the flow of urine. You will be given either a general or a spinal anaesthetic for the procedure. The operation takes about 45 minutes and you will be in hospital for about two to three days.
Open prostatectomy
When the prostate is too large to perform a TURP, it can be removed via an open incision in the lower abdomen. This is a much more radical operation than a TURP and involves a longer hospital stay and recovery period.
Greenlight laser therapy
This is a minimally invasive procedure in which the prostate is vaporised using a surgical laser, thereby clearing any obstruction it is causing to the urethra (water pipe). You will be given either a general or a spinal anaesthetic for the procedure. The operation takes about an hour and you can go home either on the same day or the next day.
UroLift®
This is a truly minimally invasive procedure that is performed as a day case, sometimes just using local anaesthetic. There is no cutting, heating or removal of prostate tissue. It involves the placement of between 2 to 4 specially designed staples into the prostate using a telescope. Two year follow up is encouraging with significant improvements in urine flow and symptoms seen. Importantly there are no sexual side effects and unlike other prostate surgery, no risk of retrograde ejaculation. It is not suitable for all prostates (large gland, large middle lobe, urinary retention), and it is necessary to perform an ultrasound and a local anaesthetic cystoscopy as part of the work up.
It is important to explore the pros and cons of these various techniques with you surgeon. The advantage of surgery is that it provides much greater symptom improvement than medication, cuts down the risks of complications from BPH, and can lead to cessation of medication. The downsides are that it involves an operation, with small complication risks, and the need for recuperation.
Prostatitis literally means inflammation in the prostate. There are several different types, which can range from a serious urological emergency to completely asymptomatic!
- Category I: Acute Bacterial Prostatitis
- Category II: Chronic Bacterial Prostatitis
- Category III: Chronic Pelvic Pain Syndrome (CPPS)
- Category IV: Asymptomatic Inflammatory Prostatitis
Prostatitis is common with a lifetime prevalence of 4-11%. It accounts for 8-12% of urologist outpatient visits, as is the most common reason for a young man to seek urological help. Quality of life with the condition can be dismal. 90% of prostatitis is category III, and maybe be nothing to do with the urinary tract. The underlying causes of this condition remain poorly understood, and treatment revolves excluding serious causes and managing symptoms as and when they arise. It is important to see an urologist in these situations.




